Meniscectomy
Authors:
Prof Leo Pinczewski MBBS, FRACS
Dr Keran Sundaraj MBBS, MSc (Trauma), FRACS, FAOA
The meniscus is a commonly injured structure in the knee. The injury can occur in any age group. In younger people, the meniscus is fairly tough and rubbery, and tears usually occur due to a forceful twisting injury. In older people, the meniscus grows weaker with age, and meniscal tears may occur due to a relatively minor injury.
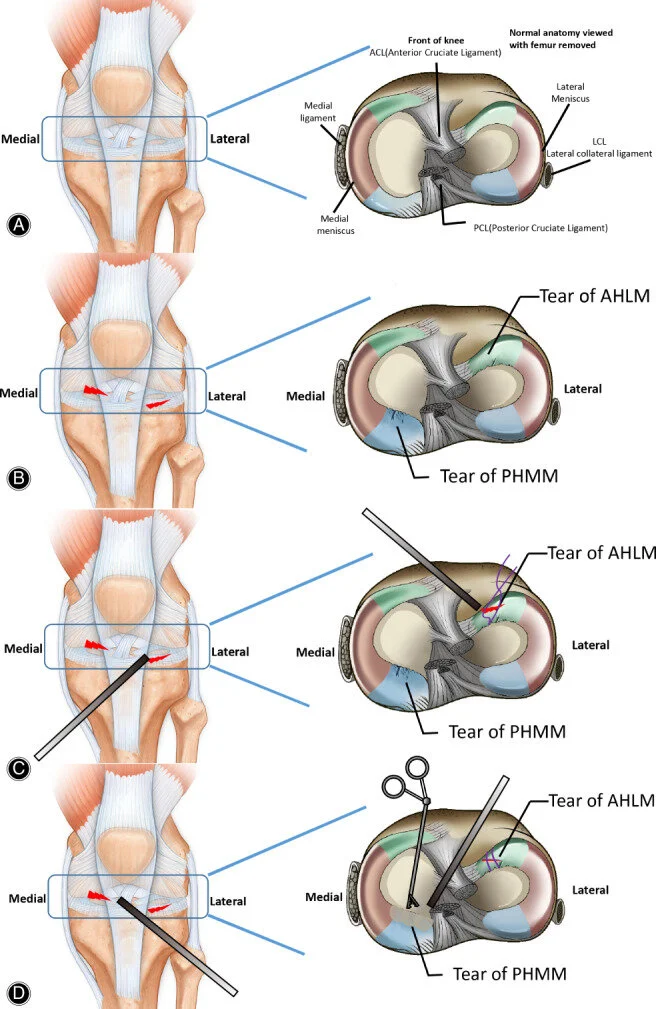
The meniscus is a half-moon shaped piece of cartilage that lies between the weight-bearing joint surfaces of the thigh and the shin and is attached to the lining of the knee joint. There are two menisci in a normal knee; the outside one is called the lateral meniscus, and the inner one is called the medial meniscus. The menisci play an essential role as a shock absorber in the knee joint, protecting the cartilage that lies on the surface of the bones from impact. The cartilage surface is a tough, very slick material that allows the surfaces to slide against one another without damage to either surface. This ability of the meniscus to spread out the force on the joint surface as we walk is important because it protects the cartilage from excessive forces occurring in any one area on the joint surface. Without the meniscus, the concentration of force into a small area on the cartilage can damage the surface, leading to degeneration over time. The menisci also cup the joint surfaces of the thigh and therefore provide some degree of stabilisation to the knee.
Aaron J. Krych, Matthew D. LaPrade, Mario Hevesi, Nicholas G. Rhodes, Adam C. Johnson, Christopher L. Camp, Michael J. Stuart (2020).Investigating the Chronology of Meniscus Root Tears: Do Medial Meniscus Posterior Root Tears Cause Extrusion or the Other Way Around?. Orthopaedic Journal of Sport Medicine. SAGE Open. doi: 10.1177/2325967120961368
Meniscal Tears
There are two different mechanisms for tearing a meniscus.
Traumatic tears result from a sudden load being applied to the meniscal tissue severe enough to cause the meniscal cartilage to fail and let go. These usually occur from a twisting injury or a blow to the side of the knee that causes the meniscus to be pushed against and compressed.
Degenerative meniscal tears are best thought of as a failure of the meniscus over time. The meniscus becomes less elastic, and complaint, and as a result, may fail with only minimal trauma (such as just getting down into a squat). Sometimes there are no memorable injuries or violent events that can be blamed as the cause of the tear.
Signs and Symptoms
The most common problem caused by a torn meniscus is pain. Patients may feel the pain along the joint line where the meniscus is located, or it may be vague and involve the whole knee. Any twisting, squatting or impacting activities will pinch the meniscus tear or flap and cause pain. Often the pain may improve with rest after the initial injury, but as soon as the aggressive activity is attempted, the pain recurs.
Swelling of the joint may occur, although meniscal tears by themselves usually don't cause a large, tensely swollen knee. Typically, low-level swelling sets in the next day after the injury and is associated with stiffness and limping.
If the torn portion of the meniscus is large enough, locking may occur. Locking refers to the inability to straighten out the knee completely. Locking occurs when the fragment of torn meniscus is caught in the hinge mechanism of the knee and will not allow the leg to straighten completely. The torn portion acts as a wedge to prevent the joint surfaces from moving.
There are long term effects of a torn meniscus as well. The constant rubbing of the torn meniscus on the cartilage may cause wear and tear on the surface, leading to joint degeneration. The knee may swell with use and become stiff and tight. This is usually because of fluid accumulating inside the knee joint.
Treatment
Initial treatment for a torn meniscus usually is directed towards reducing the pain and swelling in the knee. You may be asked to attend physiotherapy to reduce the pain and swelling and improve the range of movement. If the knee is locked and cannot be straightened out, surgery may be recommended as soon as reasonably possible to remove the torn portion that is caught in the knee joint. Once a meniscus is torn, it will most likely not heal on its own. If the symptoms continue, surgery will be required to either remove the meniscus' torn portion or repair the tear.
Surgery
Meniscal surgery is performed using the arthroscope. Small incisions are made in the knee to allow the insertion of a small camera into the joint. Through another small incision, special instruments are used to remove the torn portion of the meniscus, while the arthroscope is used to see what is happening. In some cases, the meniscus tear can be repaired using sutures. Repair of the meniscus is not possible in all cases. Young people with relatively recent meniscal tears are the most likely candidates for repair. Degenerative type tears in older people are not usually repairable.
Jun‐cheng Cui, Wen‐te Wu, Long Xin, Zhi‐wei Chen, Peng‐fei Lei (2021). Efficacy of Arthroscopic Treatment for Concurrent Medial Meniscus Posterior Horn and Lateral Meniscus Anterior Horn Injury: A Retrospective Single Center Study. Orthopaedic Surgery. SAGE Open. doi: 10.1111/os.12820
What is involved for you as the patient
Healthy patients are admitted on the morning of their surgery. You should inform your Surgeon and Anaesthetist of any medical conditions or previous medical treatment as this may affect your operation.
There must be no cuts, scratches, pimples or ulcers on your lower limb, as this dramatically increases the risk of infection. Your surgery will be postponed until the skin lesions have healed. You should not shave or wax your legs for one week before surgery.
Surgery is performed as a day procedure, and you will be leaving the hospital within hours of having your surgery performed. Overnight stay is rarely required; however, it may be necessary due to the effects of the anaesthetic or an inability to manage crutches.
Physiotherapy is commenced immediately postoperatively. A physiotherapist will supervise muscle contractions, walking and weight-bearing. Physiotherapy will continue daily following your surgery until the dressings are removed 7-10 days following surgery. Sedentary and office workers may return to work approximately 2-3 days following surgery. Most patients are walking normally within 7 days, although there is considerable patient to patient variation.
Should the left knee be involved, then driving an automatic car is possible as soon as pain allows. Should the right knee be involved, driving is permitted when you are able to walk without crutches. You must not drive a motor vehicle whilst taking strong pain relief medications.
Return to vigorous activities will be determined by the extent of the damage to your meniscus and the amount of meniscus that required removal. If minimal damage was present, then you may return to vigorous activities after 6 weeks. If significant damage was present, you may be advised to avoid impact loading activities to prevent the onset of early arthritis developing within the joint.
Potential complications related to surgery
Pneumonia: Patients with a viral respiratory tract infection (common cold or flu) should inform the Surgeon as soon as possible and have their surgery postponed until their chest is clear. Patients with a history of asthma should bring their inhalers to the hospital.
Deep vein thrombosis and pulmonary embolus: Although this complication is rare following arthroscopic surgery, a combination of a knee injury, prolonged transport and immobilisation of the limb, smoking and the oral contraceptive pill or hormonal replacement therapy all multiply to increase the risk. Any past history of thrombosis should be brought to the attention of the Surgeon prior to your operation. The oral contraceptive pill, hormonal replacement therapy and smoking should cease one week prior to surgery to minimise the risks.
Excessive bleeding resulting in a haematoma may occur with patients taking aspirin or nonsteroidal anti-inflammatory drugs - such as Voltaren, Naprosyn or Indocid. They should be stopped at least one week before surgery.
Surgery performed under strict germ-free conditions in an operating theatre. Antibiotics are administered intravenously at the time of your surgery. Any allergy to known antibiotics should be brought to the attention of your Surgeon or Anaesthetist. Despite these measures, there is a less than 1 in 300 chance of developing an infection within the joint. This may require treatment with antibiotics or, in more extreme cases, hospitalisation and arthroscopic draining of the joint with intravenous antibiotics. After such procedures, prolonged periods of antibiotics are required, and post-operative recovery is slowed.
As with all operations, if at any stage anything seems amiss, it is better to call for advice rather than wait and worry. A fever, redness or swelling around the line of the wound or an unexplained increase in pain should all be brought to the attention of the Surgeon. You can contact Dr Sundaraj by telephoning his staff during business hours or the Mater Hospital after hours. For any questions, please do not hesitate to contact our staff (02) 9437 5999. For after-hour assistance, contact Mater Hospital (02) 9900 7300.
Get in touch.
Fill out the form and one of the team will be back in touch within 24 hours.
Alternatively, give us a call on
(02) 9437 5999